Too often the liver and the GI tract are the first two organs that spring to mind when the word detoxification is mentioned. Granted, these two systems do a lot of important work in removing toxins from the body, but another vital organ that detoxifies the body are the kidneys.
The kidneys are instrumental in detoxifying a wide range of end products of metabolism. Toxins which have gone through phase II liver detoxification or direct excretion, and excess water-soluble nutrients such as B vitamins and Vitamin C are also filtered out by the kidneys (1). The kidneys allow these compounds to be removed from the body via urine, which along with stool, is the major pathway of elimination. Sweat, tears, saliva, hair, nails, and milk, all are a part of elimination as well, but to a lesser degree (2). In this blog we will discuss the kidneys and the roles they play in elimination of toxins, especially ones found on the MycoTOX Profile and the GPL-TOX Profile.
How the Kidney Works
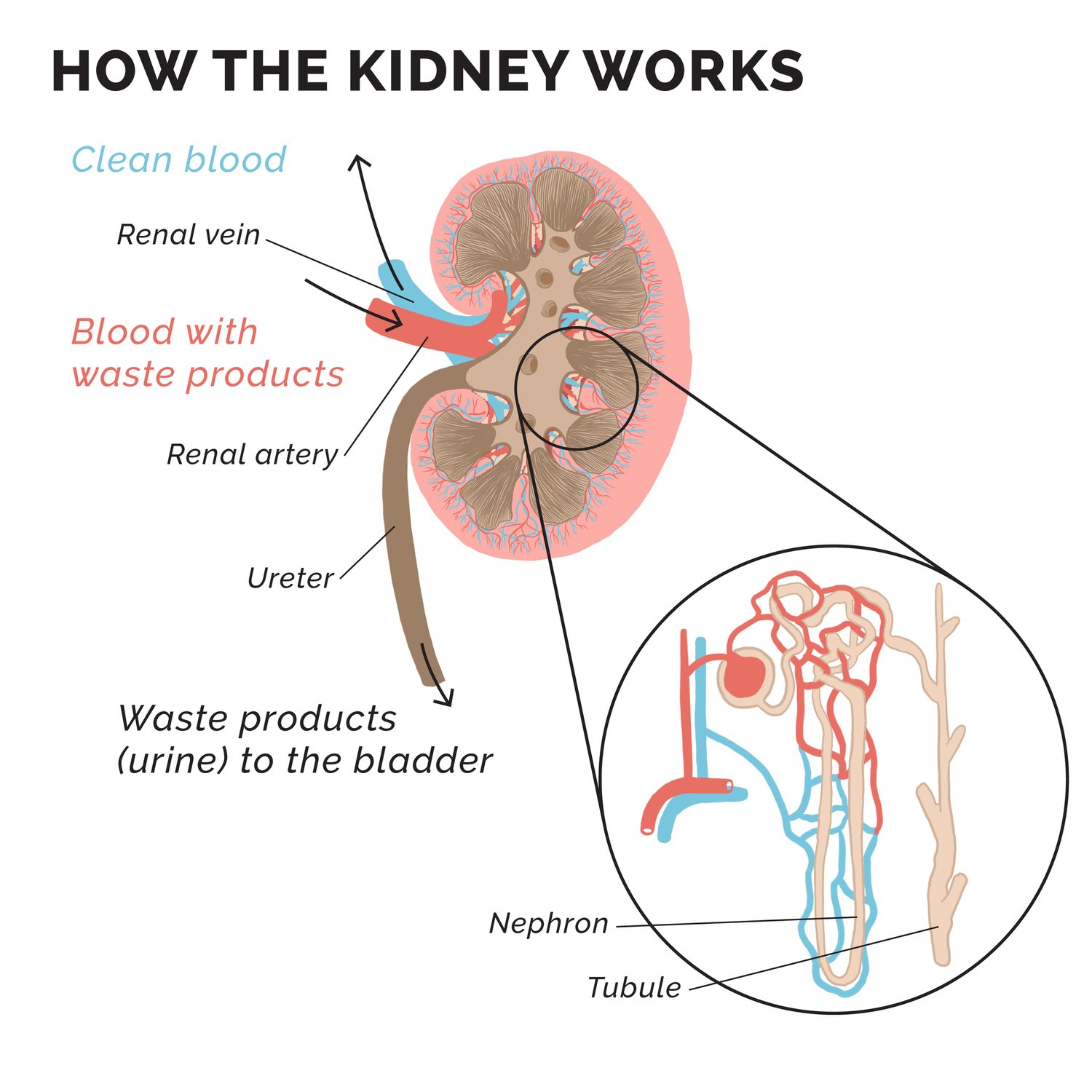
Let’s first review the kidney and its function. It is a complex, and sophisticated organ that is so important, nature felt two were necessary. These bean-shaped organs have many functions, but one of the major roles is filtering out excess water and cleaning the blood from toxins. They are so efficient, they can clean all the blood in the body in just under an hour on average (3).
The three layers of the kidney are the cortex (outer layer), medulla (inner part), and the central pelvis. Unfiltered blood travels through the cortex via the renal artery into the nephron. The nephrons are basically the blood filtering units composed of bundles of blood vessels called glomerulus, within the Bowman capsules.
When the blood passes through the glomeruli, within the medulla, waste and excess water diffuse into the capsule. The excess is then carried away by tubules to form urine, while useful substances that can be recycled are absorbed by the capillaries. The filtered blood is sent back to the heart via the renal vein. The urine is then carried through the tubules to the central pelvis, which is then emptied into two tubes called ureters, ultimately going to the bladder (2).
To be fair, the kidneys have other notable functions as well, such as release of certain hormones, stimulation of red blood cell production, and supporting fluid homeostasis within the body, but those details are outside the scope of this blog.
Eliminating Toxicants
How do toxicants enter our systems? Toxicants can be absorbed via three main pathways: respiratory tract via inhalation, integumentary system via direct skin contact, or gastrointestinal tract (GI) via consumption (2).
The pulmonary route of absorption can be quite significant as the lung tissue is highly vascularized and has a larger surface area. The GI tract also has a larger surface area, but pH has a greater influence on this systems ability to absorb.
The skin isn’t as permeable (unless there is an opening), and it’s mainly the lipid-soluble compounds that are the most worrisome, as they can be absorbed more efficiently via passive diffusion. In a very, very simplistic view, once the toxicant is absorbed via the skin or respiratory tract, it ultimately ends up in the blood where it can travel throughout the system.
The GI tract absorption is different in that if it passes through the membranes, it will likely pass through the liver before it enters general circulation. Ultimately, the body’s goal is to eliminate toxicants. As noted previously, urinary excretion via the kidney is an extremely important mechanism for this to occur.
When toxicants enter the kidney, a large amount are filtered across the glomerulus with relative ease if they are not protein bound in the plasma and/or are relatively small. Ionized toxicants tend to remain in the urine, while toxicants that are more lipophilic can re-enter renal circulation through reabsorption (2). This is the case with Ochratoxin A (OTA) from Mosaic Diagnostics’ MycoTOX Profile.
OTA is quite nephrotoxic, and this is likely because as it is going through organic anion transport in the tubules of the kidney, it is actively being reabsorbed. It is also transported with smaller carrier proteins, allowing the compound to pass through the glomerular membrane at an increased rate (5-7). Other than OTA, there are other mycotoxins that can impact the kidneys while they pass through it.
Other Ochratoxins, particularly C, can be damaging to the kidney, though the direct mechanism of action is still being investigated (8). Mycotoxins from Fusarium and Aspergillus, particularly some of the aflatoxins (B2, G1, M1 and M2), and the T2 toxin have all been documented in literature to influence the kidneys during excretion (9-12).
Evidence also indicates that Gliotoxin has cytotoxicity to renal epithelial cells, even at lower concentrations (13). Verrucarin A and Roridin E have both been found to be highly absorbed into the kidneys, even more so than the liver or lungs (14, 15).
Mycophenolic Acid (MPA) goes through glucuronidation in the kidneys, and is mainly eliminated via urine by active tubular secretion and glomerular filtration (16-18). These mycotoxins are all measured on the GPL’s MycoTOX Profile, and can be a helpful clue into what assaults are occurring on the kidneys, along with the other added benefits of running a MycoTOX Profile.
Eliminating Chemical Toxicants
Chemical toxicants passing through the kidneys can be measured in urine. The structure of the chemical compound has a large influence on its excretion through the kidneys. The more lipophilic the compound, the more likely it will be reabsorbed, or in other words, have a difficult time eliminating. The more hydrophilic compounds are, the easier they are to eliminate (1,2).
Please do not think of chemicals that are easy to eliminate as not as toxic as others. Though they may not bioaccumulate as well, the damaging effects they can have while in the system prior to elimination are still of concern, especially with chronic exposure.
Saturation plays a factor in the kidney’s ability to eliminate, meaning it only has a certain capacity it can filter. Mitochondrial function can also be a factor since the ATP generated from the citric acid cycle can help actively move the toxicants out (1).
When you look at toxicants on the GPL-TOX Profile, one can get an idea of the more water-soluble compounds by the metabolite name. If the metabolite is the same name as the parent compound, then it did not have to go through much metabolism to be eliminated. Toxicants such as Diphenyl Phosphate, Perchlorate, and 2,4-Dichlorophenoxyacetic Acid (2,4-D) all fit that description. The others are more complex, and it gets even more complex with heavy metals, but we can save that for another blog.
How to Support the Kidneys
So, we now know what the kidneys do, and what assaults can negatively impact them, the next question is how can I support it? How do we take care of the kidneys so they can do their job(s) well?
If you have been looking into the world of environmental toxins, it is abundantly clear that the most important thing to do is remove/reduce the toxicant loads. That is a whole other topic, and some really great blogs/webinars have been produced that already delve into mold testing for your body and your home as well as identifying toxins in your environment. If you don’t remove the source, no matter what you do, the problem will persist.
Additional Recommendations
Below are some additional recommendations that can be put in place to ensure our kidneys function well and are prepared to do the work of detoxification of any type of toxic intruder.
- Drinking enough clean water. Keeping fluid moving through the body and the kidneys will help them run efficiently and get the toxicants out quicker. There is no specific amount, as everyone is different, but a good general guideline is half the body weight in ounces (e.g. a 120lb person should consume around 60oz of water, minimum). Also, check the urine color to help. Too yellow means more water, clear urine means too much water, as it should have a tinge of yellow to it.
- Decrease Sodium and Phosphorus Intake. Sodium and Phosphorus in excessive amounts (not the kind in natural foods, rather the kind in processed foods) can cause imbalances in the kidneys and put additional strain on them, causing them to work harder.
- Movement. Improving blood and lymph flow through movement can help the kidneys function optimally. Walking, Yoga (added bonus with the breathing – that’s a part of detoxing too believe it or not!), bicycling, etc. Whatever movement brings joy, it will help.
- N-acetyl Cysteine (NAC). NAC has been known to protect kidneys from various assaults. A meta-analysis found that supplementation with NAC improved glomerular filtration rate and serum creatinine, indicating supportive effects (19).
- Functional Foods. Various foods can have direct effects on kidney improvement. Beets can support better blood flow throughout the system, in particular the kidneys (20). Blueberries and cabbage have been shown to help with reducing inflammation in the kidneys (21, 22). Curcumin has evidence suggesting it can be helpful in protecting the renal mitochondria (23). Cinnamon, although the effects are not directly towards the kidneys, can help control blood sugar which in turn helps support the kidneys (24).
- Be aware that some herbals can be toxic for the kidneys, while other herbs may have influences on kidney function, if the kidney is already in distress. Be mindful with herbal tinctures depending on the current state of the kidney (25).
There are other supports for the kidneys out there, but these should at least be a good start.
The kidneys are incredibly important in helping with the elimination of toxicants, and it is important to support them with lifestyle and diet. We need to support our bodies for the environment in which we live and take care of our systems to ensure they can work properly to withstand the challenges.
References: Pizzorno J. The Kidney Dysfunction Epidemic, Part 1: Causes. Integr Med (Encinitas). 2015 Dec;14(6):8-13. PMID: 26807064; PMCID: PMC4718206.Richards I and Bourgeois M. Principles and Practice of Toxicology in Public Health. 2014. ISBN: 9781449645267A, Fardon J, Friend J, Temple N, Routh, K. et al. The Amazing Body. Smithsonian. 2017. First American Edition. Pg. 154-155. ISBN: 978-1-4654-6239-8University of Michigan. Kidney Function. http://websites.umich.edu/~elements/web_mod/viper/kidney_function.htmKhoury A and Atoui A. Ochratoxin A: General Overview and Actual Molecular Status. Toxins. 2010. 2(4): 461-493. PMID: 22069596Gupta, Ramesh C. Veterinary Toxicology. Basic and Clinical Principles 3rd edition. 2018.Plumlee KH. Mycotoxins Toxicokinetics. Clinical Veterinary Toxicology. 1st Edition. 2004Abramson D. MYCOTOXINS Toxicology. Encyclopedia of Food Microbiology. 1999. Pages 1539-1547. ISBN 9780122270703. https://doi.org/10.1006/rwfm.1999.1150.Mohan J, Sheik Abdul N, Nagiah S, Ghazi T, Chuturgoon AA. Fumonisin B2 Induces Mitochondrial Stress and Mitophagy in Human Embryonic Kidney (Hek293) Cells-A Preliminary Study. Toxins (Basel). 2022 Feb 25;14(3):171. doi: 10.3390/toxins14030171. PMID: 35324667; PMCID: PMC8954924.Coppock RW, Dziwenka MM. Mycotoxins. Biomarkers in Toxicology. 2014. Pages 549-562.ISBN 9780124046306. https://doi.org/10.1016/B978-0-12-404630-6.00032-4. https://www.sciencedirect.com/science/article/pii/B9780124046306000324.Nassar AY, Megalla SE, El-Fattah HM, Hafez AH, El-Deap TS. Binding of aflatoxin B1, G1 and M to plasma albumin. Mycopathologia. 1982 Jul 23;79(1):35-8. doi: 10.1007/BF00636179. PMID: 6811900.Adhikari M, Negi B, Kaushik N, Adhikari A, Al-Khedhairy AA, Kaushik NK, Choi EH. T-2 mycotoxin: toxicological effects and decontamination strategies. Oncotarget. 2017 May 16;8(20):33933-33952. doi: 10.18632/oncotarget.15422. PMID: 28430618; PMCID: PMC5464924.Gayathri, L., Akbarsha, M. & Ruckmani, K. In vitro study on aspects of molecular mechanisms underlying invasive aspergillosis caused by gliotoxin and fumagillin, alone and in combination. Sci Rep 10, 14473 (2020). https://doi.org/10.1038/s41598-020-71367-2Amuzie CJ, Islam Z, Kim JK, Seo JH, Pestka JJ. Kinetics of satratoxin g tissue distribution and excretion following intranasal exposure in the mouse. Toxicol Sci. 2010;116(2):433-440. doi:10.1093/toxsci/kfq142Amuzie CJ, Islam Z, Kim JK, Seo JH, Pestka JJ. Kinetics of satratoxin g tissue distribution and excretion following intranasal exposure in the mouse. Toxicol Sci. 2010;116(2):433-440. doi:10.1093/toxsci/kfq142Food and Drug Association. Mycophenolic acid (Myfortic). https://www.accessdata.fda.gov/drugsatfda_docs/label/2008/050791s002lbl.pdfLamba V, Sangkuhl K, Sanghavi K, Fish A, Altman RB, and KE.PharmGKB. Mycophenolic Acid Pathway. Pharmacogenetics and genomics.2014. PMID:24220207. https://www.pharmgkb.org/pathway/PA165964832Hooijmaaijer E, Brandl M, Nelson J, Lustig D. Degradation products of mycophenolate mofetil in aqueous solution. Drug Dev Ind Pharm. 1999 Mar;25(3):361-5. doi: 10.1081/ddc-100102183. PMID: 10071831.Ye M, Lin W, Zheng J, Lin S. N-acetylcysteine for chronic kidney disease: a systematic review and meta-analysis. Am J Transl Res. 2021 Apr 15;13(4):2472-2485. PMID: 34017406; PMCID: PMC8129408.Kolluru GK, Kevil CG. Beets, bacteria, and blood flow: a lesson of three Bs. Circulation. 2012 Oct 16;126(16):1939-40. doi: 10.1161/CIRCULATIONAHA.112.136515. Epub 2012 Sep 19. PMID: 22992323; PMCID: PMC4078643.Nair AR, Masson GS, Ebenezer PJ, Del Piero F, Francis J. Role of TLR4 in lipopolysaccharide-induced acute kidney injury: protection by blueberry. Free Radic Biol Med. 2014 Jun;71:16-25. doi: 10.1016/j.freeradbiomed.2014.03.012. Epub 2014 Mar 19. PMID: 24657730.Asiwe JN, Kolawole TA, Anachuna KK, Ebuwa EI, Nwogueze BC, Eruotor H, Igbokwe V. Cabbage juice protect against lead-induced liver and kidney damage in male Wistar rat. Biomarkers. 2022 Mar;27(2):151-158. doi: 10.1080/1354750X.2021.2022210. Epub 2022 Jan 3. PMID: 34974788.Trujillo J, Chirino YI, Molina-Jijón E, Andérica-Romero AC, Tapia E, Pedraza-Chaverrí J. Renoprotective effect of the antioxidant curcumin: Recent findings. Redox Biol. 2013 Sep 17;1(1):448-56. doi: 10.1016/j.redox.2013.09.003. PMID: 24191240; PMCID: PMC3814973.Khan A, Safdar M, Ali Khan MM, Khattak KN, Anderson RA. Cinnamon improves glucose and lipids of people with type 2 diabetes. Diabetes Care. 2003 Dec;26(12):3215-8. doi: 10.2337/diacare.26.12.3215. PMID: 14633804.National Kidney Foundation. Use of Herbal Supplements in Chronic Kidney Disease. 2009. https://kidneyhi.org/use-of-herbal-supplements-in-chronic-kidney-disease/